GASTROSOPHAGEAL REFLUX (HEARTBURN)
What is reflux ?
Intermittently the usually acidic contents of the stomach can ascend into the oesophagus causing irritation of the inner (mucosal) lining of the oesophagus. (oesophagitis) Classic symptoms include heartburn, regurgitation and a sour taste. Night cough, asthma, sore throat and ear pain may also be caused by reflux.
What is the cause of reflux ?
In most cases the sphincter (valve) at the stomach entrance is no longer watertight and allows fluid from the stomach to ascend into the oesophagus for prolonged periods. Furthermore the upper portion of the stomach often ascends into the chest, an anomaly which is known as a hiatal hernia.
How efficient are drugs in treating reflux ?
Antiacids constitute the first line of treatment for reflux. By reducing the acidity of the reflux they alleviate symptoms and cure oesophagitis in 90% of patients. Medications are however unable to reinforce the sphincter or repair the hiatal hernia and in fact patients continue to have reflux that is less irritating because no longer acidic. Antiacids usually cannot be discontinued because symptoms and oesophageal irritation reappear within one year in 80% of patients.
Why consider surgery ?
Discouraged patients whose quality of life is impacted by long-standing reflux are eventually referred to a surgeon, often after months or even years of drug treatment. Surgery can be of aid particularly in the following situations:
- Incomplete relief of heartburn with drug therapy
- Recurrence of symptoms at cessation of treatment
- Patient reluctance to take medications lifelong
- Severe and complicated forms of oesophagitis
- Symptoms not improved by drugs (asthma, night cough)
What does surgery entail ?
Surgery is all the more attractive that it is performed by a minimally invasive approach (keyhole) and takes 1 hour to perform, causes moderate pain postoperatively and involves just a 2-3 day hospital stay. Transient schoulder pain lasting several hours is common and due to the presence of residual air within the abdomen. The patient can resume normal activities immediately but should avoid strenuous physical exercise for 6 weeks. A semi-liquid diet is prescribed for 2-3 weeks. Two months postoperatively the vast majority of patients claim a spectacular improvement of their quality of life and the long-term success rate is 90%.
 |
 |
|
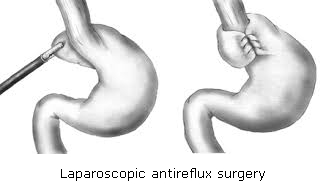
| FIG : Operative setup and trocar sites. Source : P Hauters,C Bertrand,M Legrand,E van Vyve,J Closset Traitement chirurgical du reflux gastroœsophagien de l’adulte EMC-Techniques chirurgicales-Appareil digestif 2014 ;9(4) :1-17 Article 40-188 | FIG 1 : Antireflux valve creation Source: James P. Gray, M.D. 2007 : |
Are there side-effects ?
A feeling of ‘tightness’ or even transient food impaction in the lower chest is common, lasting 2-3 weeks. Patients are advised to eat slowly semi-liquid meals in a calm environment during that period. Later solid foods should be chewed thoroughly. Bloating after meals, accompanied by fullness, early satiety and nausea sometimes occurs and is linked to a reduction in belching. Postoperatively a durable increase in flatulence is common. Avoid sparkling fluids and talking while eating.
Vomiting is usually no longer possible. In case of nausea it is advised to take Motilium Instant sublingually or ondansetron (Zofran) suppository. Avoid trying to make yourself vomit.
Despite these inconveniences a large majority of patients can expect spectacular improvement in their quality of life and 90% long-term relief. It is revealing that many patients have just one regret, that of not having been offered surgery earlier.
Dr Serge Landen - www.drlanden.be