COLONIC AND RECTAL SURGERY
The colon and rectum (large bowel) are affected by inflammatory and tumoral processes that may require surgery. The resulting bowel paralysis during the first 4-5 postoperative days is a cause of abdominal bloating and significant discomfort. A variety of measures are now taken to improve patient comfort without compromising safety:
- Colonic preparation using laxatives is no longer performed routinely
- Nasogastric tubes are becoming redundant
- Early postoperative oral intake is standard
- Patient controlled analgesia is tailored to the patient’s needs
- Less postoperative pain allows early mobilisation
- Minimally invasive surgery decreases postoperative discomfort and disability
Applying these measures selectively I have been able to reduce the length of hospital stay by one half during the last decade.
The rectum is the terminal portion of the colon situated directly above the anus. Because the rectum is sited deeply within the pelvis tumours at this level can be difficult to remove without sacrificing nerve structures and possibly the anal sphincter. Significant progress has been accomplished to increase curability whilst decreasing permanent disabilities:
- Accurate preoperative staging modalities including magnetic resonance and endoscopic ultrasound are capable of selecting early stage tumours amenable to local resection through a transanal route as well as identifying more advanced tumours that will benefit from preoperative radiochemotherapy prior to surgery.
- Patients with advanced rectal tumours receive a 5-week course of radiochemotherapy 6-8 weeks before surgery, making the latter easier and decreasing local recurrences.
- Meticulous surgical en-bloc dissection of the rectum and surrounding fat remains however the single most important factor to reduce local recurrence.
- Meticulous surgical technique can often avoid nerve trauma within the pelvis and avoid significant disability of urinary and sexual functions.
- Preservation of the anal sphincter (avoidance of a permanent stoma) is the standard even for low-lying tumours.
 |
|
|
|
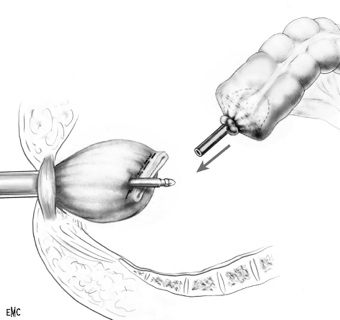
FIG: Minimally invasive colectomy; Source: I Pirlet N Mercier,JM Fabre Traitement chirurgicale des cancers du colon gauche EMC-Techniques chirurgicales-Appareil digestif 2013;8(4):1-10 Article 40-572)
|
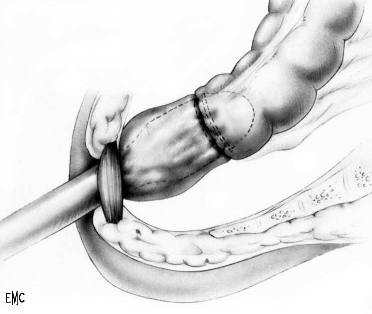
FIG: Stapled anastomosis: connecting colon and rectum |
FIG: Finished anastomosis before removal of stapler. Source: L de Calan,B Gayet,P Bourlier,T Perniceni Chirurgie du cancer du rectum par laparotomie et par laparoscopie EMC-Techniques chirurgicales-Appareil digestif 2004:1-30 Article 40-630 |
Colonic diverticula are very common in older patients. Diverticular inflammation (diverticulitis) occurs in a quarter of these and according to severity symptoms range from left lower quadrant pain to diffuse abdominal guarding and peritonitis.
Until recently diverticular peritonitis required a two-staged approach calling for urgent surgery and a colostomy followed 3-8 months later by a second major operation to restore intestinal continuity. Without increasing the risk for the patient I promoted a single stage operation that avoids the disability of a temporary stoma and the need for a second operation. This strategy has become popular because it also significantly reduces hospitalization time and costs.*
|
|
|
Dr Serge Landen - www.drlanden.be